It is estimated that at least 3.6% of America’s adult population suffers from post-traumatic stress disorder (PTSD). That means one in every 11 adults and some adolescents will be diagnosed with this mental health disorder in their lifetime.
PTSD to this day is still heavily associated with war veterans, as it was initially used as a diagnosis among soldiers returning from World Wars I and II. Today, the mental health community is aware that anyone can develop PTSD.
While most people suffering from PTSD are typically put on a regimen of antidepressants and talk therapy, these methods are known to fail almost as much as they’re known to bring relief.
Now mental health professionals are turning to Transcranial Magnetic Stimulation (TMS) as a more promising form of treatment when all other options fail.
To learn more about PTSD and TMS as a potential treatment, keep reading.
PTSD: What Makes it Different?
When someone lives through a traumatic event, such as active combat, assault, an open-shooter situation, or even a natural disaster, they’ll likely exhibit the symptoms and signs associated with anxiety afterward.
Event-related anxiety symptoms tend to subside as time passes. However, when it comes to PTSD, these symptoms actually worsen over time.
What separates PTSD from other stress disorders, like anxiety, is the fact that it affects each area of the brain in a way that causes it to become overly sensitive and therefore easily triggered.
The result is that the area of the brain responsible for thinking and memory – the frontal lobe – stops functioning properly. When this happens, it becomes harder to separate the safety of the events happening in the now from the traumatic events that occurred in the past.
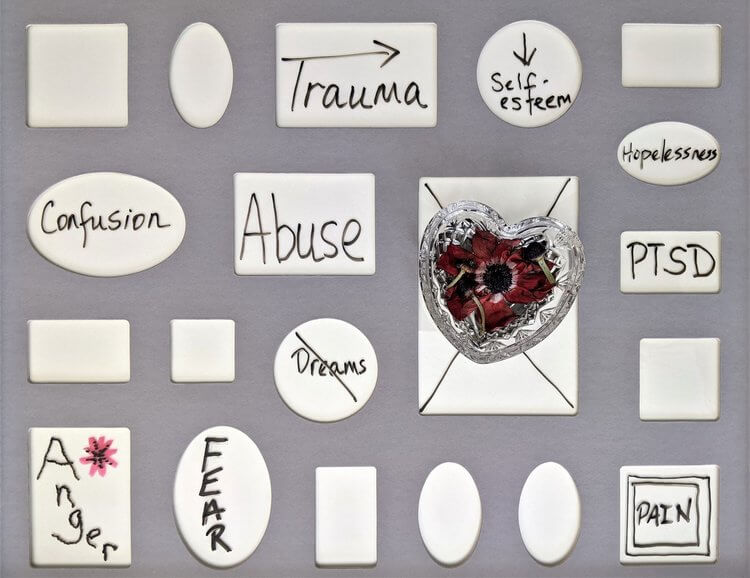
Therefore, PTSD is typically characterized by the following:
- Intrusive thoughts that are persistent and distressing, such as hyperrealistic memories, flashbacks, and even nightmares
- Avoidance behaviors, where the individual will purposefully avoid places and situations that can trigger intrusive thoughts
- Negative thought patterns, which constantly plague the individual with emotions such as anger, fear, guilt, or shame—often causing distrust in family and friends
- Heightened arousal, which often leads to irritability and angry outbursts. When severe, it can lead to reduced concentration, self-destructive behaviors, and substance abuse
All of the above can get to the point where the individual begins to detach from their loved ones and even reality.
While antidepressants often benefit individuals suffering from PTSD, with a response rate of 60%, only between 20% and 30% achieve full remission.
TMS and PTSD
When it comes to treatment-resistant mental health disorders, TMS is becoming the next best option in the eyes of mental health professionals.
TMS is non-invasive, safe, and painless, and it works by stimulating certain areas of the brain as a means to “rewire” them – or, alter the brain’s patterns to return them to normal in terms of thoughts and behaviors.
This rewiring has proven effective at alleviating the symptoms associated with anxiety and depression and is currently approved by the FDA for the two mood disorders.
Recent studies have found that TMS proved to be effective at improving the symptoms of PTSD in study participants who exhibited both major depressive disorder (MDD) and PTSD.
While TMS as a treatment for PTSD has not yet been FDA-approved, there are indications that it’s well on its way as a secondary approach for treatment-resistant PTSD and other mental health disorders.
Visit our site to learn more about TMS as a treatment or to view the other services we offer for mental health and wellness.